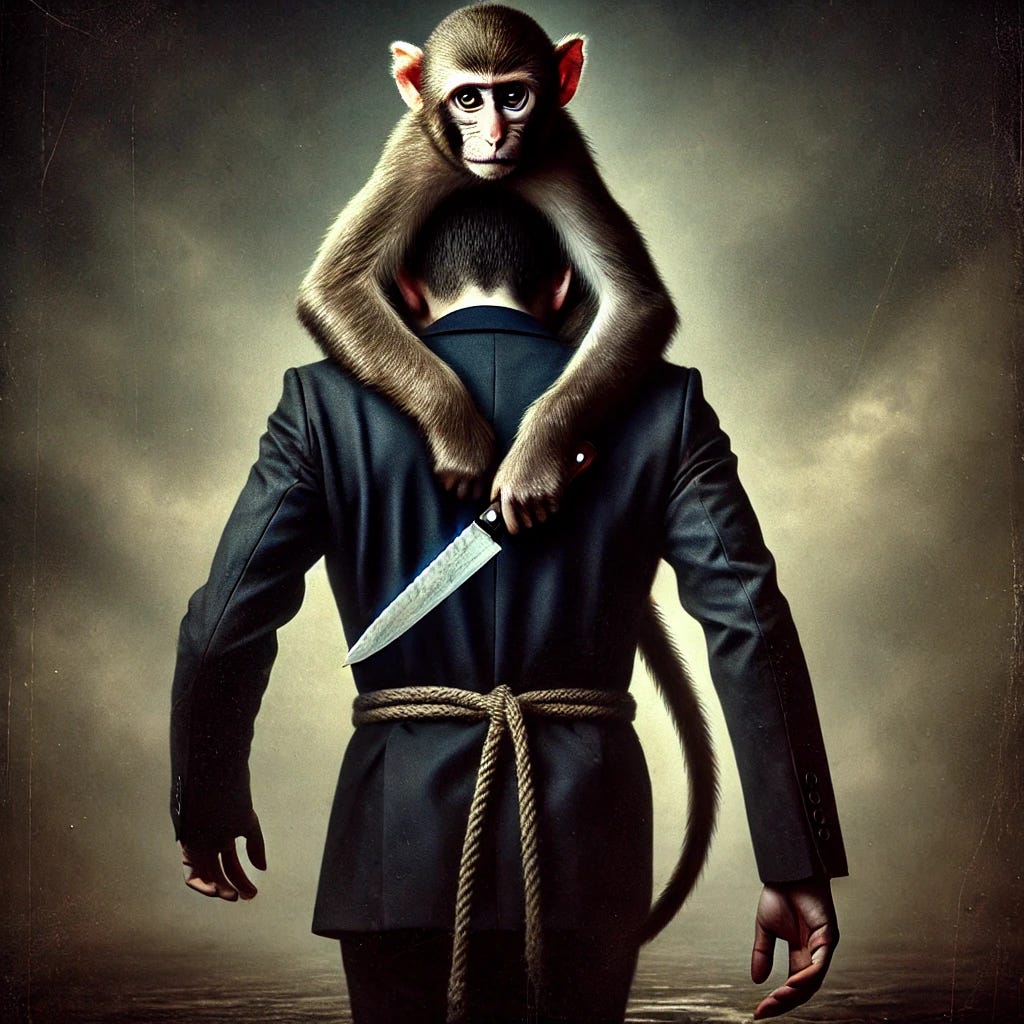
I often say that lumbar spinal fusion for back pain management is the lobotomy of our time. Why?
First, spinal fusion was never designed as a procedure to eliminate pain. It was originally developed to stabilize the spine after severe trauma and prevent neurological damage. Somewhere along the way, in the 1990s, surgeons began experimenting with its use for pain management.
Make no mistake—back pain, which affects nearly all of us, can be excruciating, frustrating, and leave many feeling hopeless. Desperate for relief, patients often encounter surgeons who suggest that spinal fusion will not only help but also prevent future damage. Unfortunately, this is false.
Multiple randomized controlled trials have shown that, in terms of pain and disability, there is no significant difference in outcomes between those with chronic low back pain who undergo lumbar fusion and those who follow a non-surgical approach. The difference? Patients who undergo fusion surgery face higher rates of infection, drug dependence, subsequent surgeries, and even death compared to those who choose non-surgical treatments.
Yet, despite the evidence, spinal fusions continue to be performed at alarming rates. In the United States, the number of spinal fusions has been steadily increasing. In 2021 alone, approximately 1.36 million instrumented spinal procedures were performed.
There are situations where spinal fusion may be appropriate—such as for significant trauma resulting in neurological loss or, in some cases, severe lumbar spondylolisthesis though even this remains controversial (more on this in a future post). However, if lumbar spinal fusion is being recommended to you for chronic back pain, you should be highly skeptical. Seek multiple opinions from both surgeons and non-surgeons, and fully understand the risks and benefits before making a decision.
In the end, the choice is yours. Own your health.